Seizures may occur after traumatic brain injury; these are known as post-traumatic seizures (PTS). However, not everyone who has post-traumatic seizures will continue to have post-traumatic epilepsy (PTE), because the latter is a chronic condition. However, the terms PTS and PTE are used interchangeably in medical literature.
Understanding epilepsy and seizures
Post-traumatic epilepsy is defined as two or more seizures, thought to be related to the injury itself, that follow a traumatic injury occurring later than one week following the injury.
Patients with traumatic brain injury (TBI) are at higher risk for the development of epilepsy relative to the general population.
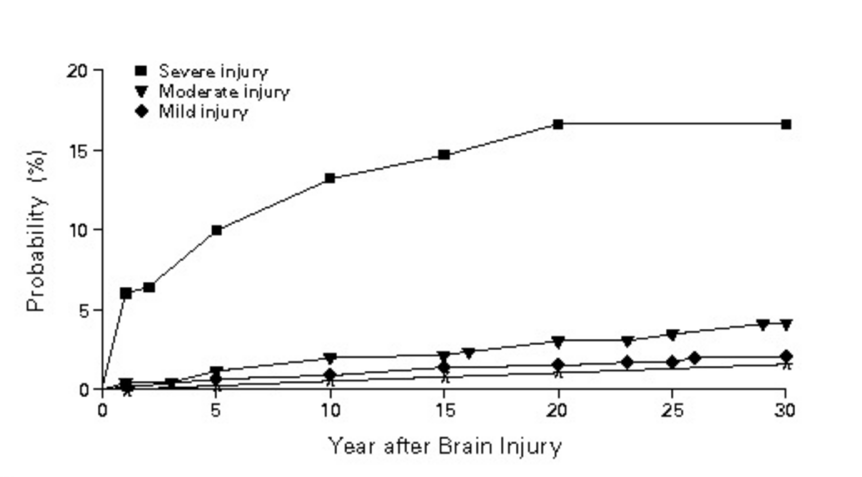
As for the statistical likelihood of epilepsy in TBI patients, reports propose varying ranges with many resting anywhere from 3-20 % dependent on the severity of injury, which if severe, could increase the potential to approximately 40%.
Results from the most often quoted study for the cumulative probability of unprovoked seizures (1) are summarised below.
PTE ranges from simple partial, complex partial to secondarily generalised seizures.
The definitions of each, from the Epilepsy Foundation are as follows:
- – simple partial seizures, usually lasting around 2 minutes, is characterised as either motor, sensory, autonomic or psychic seizures in which the individual is usually alert
- – complex partial seizures, lasting 1 to 2 minutes, include automatisms (such as lip smacking) in which the individual is unaware of their surroundings
- – secondarily generalised seizures begin in one area of the brain, and spread to both hemispheres lasting anywhere from 1-3 minutes, these seizures are convulsive and it can take much longer for the patient to recover.
Factors such as age, previous seizures, smoking, genetics, timing of seizures and types of injury, all play a role in the potential for the development of PTE.
Age plays a role in the latency period of seizures following TBI. In one study a latency period of around 3 years existed in those who were over 14 while there was an 18 year latency period in those who were 2 years or younger at the time of the trauma.
Categorising seizures after brain injury
Seizures following TBI are classified into three categories: immediate, early and late onset.
- – Immediate onset seizures occur within 24 hours following the injury
- – Early onset seizures typically occur less than a week after injury and are often seen as a precursor for late seizures.
- – Late onset seizures are found to occur more than a week after the injury and have been seen to occur for years following. These late seizures appear to increase the likelihood for PTE.
When comparing early versus late onset seizures, the different risk factors associated with each have been identified.
Understanding risk factors
- – Risk factors for early onset seizures comprise: acute intracerebral hematoma, acute subdural hematoma, younger age, increased injury severity, and chronic alcoholism.
- – Risk factors for late onset seizures include early posttraumatic seizures, brain contusion, subdural hematoma, prolonged post-traumatic amnesia (> 3 days), increased injury severity, depressed skull fracture and older than 65 years of age at the time of injury.
Most notable of all the previous risks, is the severity of the injury itself. Common clinical markers of head injury severity include the Glasgow Coma Score, length of posttraumatic amnesia, length of loss of consciousness, extent of brain damage and brain volume loss shown on CT scan.
The relative risks (RRs) for developing epilepsy after various brain insults have been summarised in the chart below.
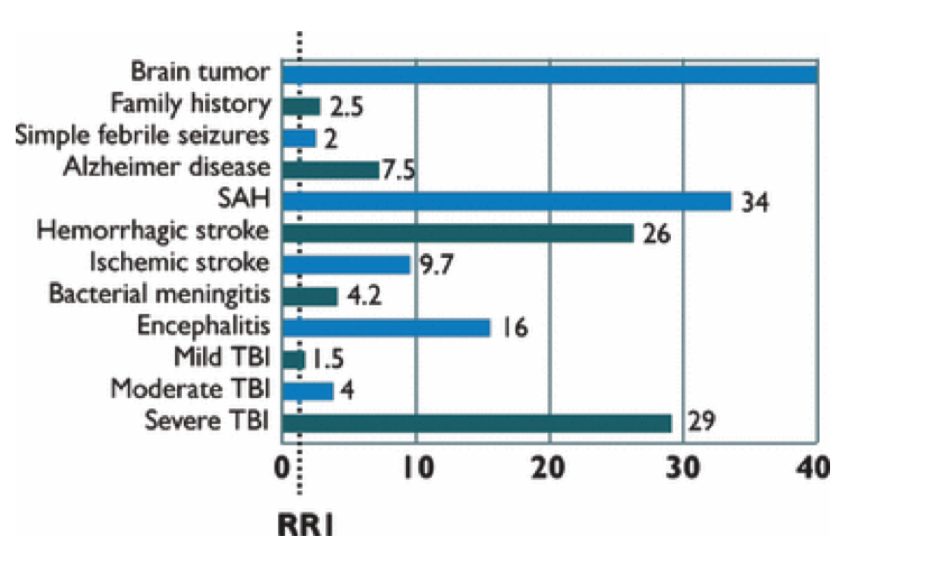
As shown patients with severe TBI have a 29‐fold increased risk of developing epilepsy compared to the general population. This RR is exceeded only by brain tumor (RR = 40) and subarachnoid hemorrhage (RR = 34). Not surprisingly, the RR for epilepsy after TBI is strongly related to the severity of head injury. There is a 4‐fold increased risk after moderate TBI and only a 1.5‐fold increased risk after mild TBI.
What kind of brain injury causes epilepsy?
Penetrating versus closed head injuries damage the brain differently, leaving an altered likelihood for PTE. While closed head injuries often lead to axonal tearing, diffuse oedema and ischemia, causing the release of excitatory amino acids and other toxic chemicals that can cause additional damage, penetrating injuries produce a cicatrix (the scar of a healed wound) in the cortex, increasing the likelihood of PTE to about 50% versus 30% for the closed head injuries.
Late seizures, which have been noted as a risk factor for epilepsy, are seen to be due to the damage of the cortex by free radicals that have been generated following the deposit of iron and the increased toxic level of glutamate.
Studies have also proposed that the reorganization of the circuitry in the brain can lead to epileptogenesis which is defined as the process by which a non-epileptic brain transforms into one that produces unprovoked seizures through the development of brain tissue capable of seizures.
Diagnosis, treatment and managment of epilepsy
Current lines of treatment are structured in a step-wise process beginning with Anti-Epileptic Drug (AED) treatment, then moving to resection surgery if AED treatment is not ultimately effective and on to vagus nerve and deep brain stimulation for medically refractory epilepsy.
While seizure prophylaxis can prevent early onset seizures, no available treatments effectively prevent late-onset seizure.
To be diagnosed with PTE, a person must have a history of head trauma and no history of seizures prior to the injury. Witnessing a seizure is the most effective way to diagnose PTE.
Electroencephalography (EEG) is a tool used to diagnose a seizure disorder, but a large portion of people with PTE may not have the abnormal “epileptiform” EEG findings indicative of epilepsy.
EEG can be useful to localize the epileptic focus, to determine severity, and to predict whether a person will suffer more seizures if they stop taking antiepileptic medications.
It is frequently not possible to detect the epileptic focus using neuroimaging (MR and CT).
For a diagnosis of PTE, seizures must not be attributable to another obvious cause. Seizures that occur after head injury are not necessarily due to epilepsy or even to the head trauma. Like anyone else, TBI survivors may suffer seizures due to factors including imbalances of fluid or electrolytes, epilepsy from other causes, hypoxia (insufficient oxygen), and ischemia (insufficient blood flow to the brain).Withdrawal from alcohol is another potential cause of seizures. Thus these factors must be ruled out as causes of seizures in people with head injury before a diagnosis of PTE can be made.
The impact of epilepsy on life expectancy
People with PTE are thought to have shorter life expectancies than people with brain injury who do not suffer from seizures.
The results of one study (2) indicate that individuals with late post-traumatic seizures (LPTS) in the first two years post-TBI have a very high mortality rate at a younger age compared to individuals with TBI and no LPTS and those with epilepsy in general. Even without adjusting for age, those with TBI and LPTS have nearly three times the mortality rate of those with TBI alone, 27% versus 10% in this study. They die 15 years younger than those who have TBI alone, but do not differ significantly in duration post-TBI or in initial severity of injury as measured by GCS or the severity of mid-line shift.
Compared to people with similar structural brain injuries but without PTE, people with PTE take longer to recover from the injury, have more cognitive and motor problems, and perform worse at everyday tasks. This finding may suggest that PTE is an indicator of a more severe brain injury, rather than a complication that itself worsens outcome. PTE has also been found to be associated with worse social and functional outcomes but not to worsen patients’ rehabilitation or ability to return to work. However, people with PTE may have trouble finding employment if they admit to having seizures, especially if their work involves operating heavy machinery.
References
- A Population-Based Study of Seizures after Traumatic Brain Injuries: John F. Annegers, Ph.D., W. Allen Hauser, M.D., Sharon P. Coan, M.S., Walter A. Rocca, M.D., M.P.H.: N Engl J Med 1998; 338:20-24
- Mortality in Late Post-Traumatic Seizures: Jeffrey Englander, Tamara Bushnik, Jerry M. Wright, Laura Jamison,and Thao T. Duong: J Neurotrauma. 2009 Sep; 26(9): 1471–1477.